‘This disease is just crushing communities of color’: Emergency room doctors on how COVID-19 is laying bare inequities in health care
“This is not only exposing how the system fails patients, but it is also exposing how the system fails providers.”

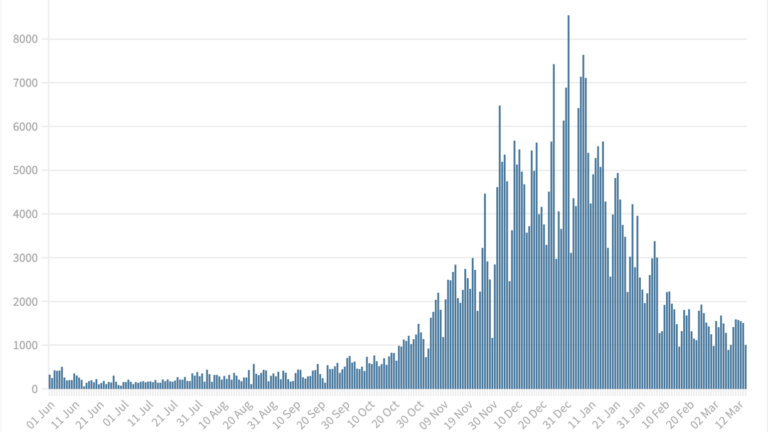
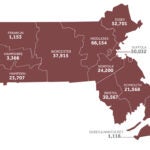
As the coronavirus pandemic continues to rage in Massachusetts, more evidence emerges each week that the virus is disproportionately affecting the state’s communities of color.
Related Links
The Massachusetts Public Health Association released a review of the state’s reported coronavirus cases on Wednesday that revealed the rate of infections for Latinx residents in Massachusetts is three times that of white residents. Black residents are seeing two-and-a-half times more infections per capita than white residents.
The public health nonprofit is just the latest group to call for urgent action by Gov. Charlie Baker and state officials to address the health inequities and disproportionate impacts the pandemic has had on vulnerable populations in Massachusetts.
“While there are still gaps in the data that should be addressed, we have enough data to say with a high degree of confidence that Black and Latinx residents of Massachusetts are suffering from COVID-19 infections at rates far higher than Whites,” Carlene Pavlos, executive director of the association, said in a statement. “The Baker Administration should release data in a way that makes this reality clear, and more importantly, should act aggressively and urgently to address these staggering inequities.”
(2/2) “The Baker Administration should release data in a way that makes this reality clear, and more importantly, should act aggressively and urgently in the face of these staggering inequities.” View the full release here: https://t.co/B60twOlm5a
— MA Public Health Association (@MAPublicHealth) April 22, 2020
Signs of the alarming trend — that the coronavirus pandemic was hitting poor communities and communities of color hard in the Boston area — were present a month ago, according to Alister Martin, an emergency room doctor at Massachusetts General Hospital.
“So many of our patients needing ventilators today were from Boston’s lower [socioeconomic status] communities,” he wrote on Twitter in late March. “The pandemic has put our inequities on full display. There will be a post COVID and our healthcare system needs to learn the lessons from it and be re-made to work for everyone.”
Weeks later, Martin’s concerns about what he’s seeing at his hospital remain the same.
“This disease is just crushing communities of color,” he said in a recent interview with Boston.com. “By far the majority of patients that we are seeing that are really, really, really sick COVID patients are Hispanic at Mass. General. The population of Latinx folks in Boston is somewhere around 15 to 17 percent and nearly 50 percent of the people in our hospital right now, in beds in the ICU or on the floor who have COVID, are Hispanic.”
In Boston, Hyde Park, Dorchester, and East Boston were among the city’s neighborhoods with the highest rates of infections, according to the latest information available from the city’s public health commission.
Factors for why the pandemic is impacting already vulnerable communities all have to do with poverty and inequities that existed before the virus appeared, advocates and health care providers agree.
“So much of a person’s health, even pre-COVID-19, is related to the zip code they live in,” state Rep. Jon Santiago, who works in the emergency room at Boston Medical Center, told Boston.com in a recent interview. “Things like poverty and trauma and lack of educational opportunities, all things that define these communities, will inevitably result in poor health outcomes. And that’s what was there long before COVID-19. All COVID-19 has really done is expose that to the person who maybe wasn’t paying attention before.”
Wow. The disparities are concerning and I can’t say surprising. #Covid19 has not just exposed but exacerbated them. Great work @ckelly60637 @sagarm91 @DocMcStewson! pic.twitter.com/NwHLMV9tZW
— Jon Santiago (@IamJonSantiago) April 21, 2020
For low-income individuals or those experiencing poverty, it is often harder to follow the guidelines to self-isolate and quarantine if they fall ill because of their living situations. The same individuals may also be working essential jobs and are financially unable to stay home in the first place to avoid exposure to the virus.
“People don’t have a study in their apartment where they can just camp out while the rest of the family doesn’t interact with them — they don’t have a downstairs basement to keep themselves away from an elderly grandma who lives upstairs,” Martin said. “In fact, what they have is what I’ve seen almost a half dozen times now — a working-class, middle-aged woman who’s got several kids comes into the hospital with COVID symptoms, has COVID, and lives at home in a one bedroom in Dorchester with her elderly mother and her three kids. And when I tell her that she has COVID and she needs to self-isolate, she says, ‘How am I supposed to do that? What does that mean for me?’”
As it stands, Martin said he and his colleagues are left with no way to answer that question for patients.
“This is not only exposing how the system fails patients, but it is also exposing how the system fails providers,” he said.
Separate of the moral obligation to address those gaps for vulnerable populations, the emergency room physician warned the impact of recurring clusters of infections in poor communities will mean resurgences of the virus in years to come.
“We need to figure this out, and we need to create systems that allow us to really address the folks who are most vulnerable, because if they keep getting reinfected then we’re all screwed,” Martin said.
So far, some steps have been taken to address concerns about health disparities in the middle of the pandemic. In response to concerns about equity raised by advocates, health care workers, and politicians, state officials revised guidelines for how ventilators can be rationed. Previously, the guidelines recommended use of a priority scoring system to assess patients that factored in co-morbid conditions.
Critics of those initial guidelines, which included Martin and Santiago, argued that the recommendations would have disproportionately impacted patients with disabilities and patients of color, given longstanding health care and socioeconomic disparities mean those communities are more likely to suffer from co-morbid illnesses.
Proud to see physicians, social workers, nurses, and healthcare providers on the front line across 5 major Boston hospitals come together and speak out on how the crisis standards of care guidelines could disproportionately impact black and brown communities. Our press release pic.twitter.com/jAhtzaUgBe
— Alister Martin (@AlisterFMartin) April 13, 2020
The change was a step in the right direction, according to Martin, but the doctor argued before the Boston City Council’s Public Health Committee on Wednesday that more can be done to address inequities in health care.
Pointing to how the outbreak unfolded in Chelsea, Santiago said communities of color should be considered as vulnerable and potential hotspots before infections occur and action should be taken, in the same way that the state has moved to address cases in nursing and long-term care homes. Interventions for people to easily get tested, care, and information about the virus should be proactive in cities across the state like Lynn, Lawrence, and Springfield, he said.
“For many of us working already on the ground, on the front line, we knew the disparities were going to be there,” he said. “And our experiences on the front lines suggest that they are there … Chelsea will not be the last minority community that’s going to be hit hard by this epidemic.”
Increasing the availability of testing, both Martin and Santiago emphasized, is a critical step. State officials announced this week they were expanding testing at community health centers as a means of trying to address the emerging clusters of infections.
“Community health centers provide comprehensive health services for people across the commonwealth,” Baker said during a press conference on Wednesday. “And these facilities are also deeply rooted in the fabric of their local communities. They’re trusted partners in addressing the broad health needs of underserved populations, and they’re committed to eliminating health disparities and facilitating access to health care for those they serve.”
Santiago added that it is important for those involved in the contact tracing efforts to be representative of the communities they’re working with and for there to be an emphasis on culturally competent health services. Existing leadership in minority communities should also be tapped by the state for involvement in the coronavirus response, he said.
The two emergency room physicians say the pandemic — in exposing so clearly the disparities — presents a tremendous chance to create change.
For the first time, Martin said, many people are seeing how inequitable the health care system is in a way they hadn’t been exposed to before.
A month ago, he recalled, patients were coming into the hospital seeking tests for the coronavirus, only to be told the tests weren’t available for them.
“They’re like, ‘What do you mean you don’t have any tests? I just saw the entire Brooklyn Nets basketball team got tested, what do you mean you don’t have any tests?’” Martin said. “That should tell you everything you need to know about our system. You start to get who the winners and losers are in our system with that fact alone. And often people who are living comfortably don’t get to see the cracks in the health care system and because of this, they were. For some people, they were really brought to this new realization of how messed up things are.”
Both physicians said they are encouraged by how physicians and local leaders alike have raised awareness and made moves to address the disproportionate impacts of the pandemic. The ongoing advocacy and discussions make them hopeful that more change is possible to address the longstanding inequities and prevent the situations that have arisen with the coronavirus from repeating during the next public health crisis.
“Not just with respect to these longstanding health inequities, but just whether we should tie health care to employment, whether we should be more aggressive when it comes to addressing housing insecurity and all the issues that come with that,” Santiago said. “I think this is a prime moment … what can we do to put ourselves in a position to live in a fair, more just society? So with the next crisis we won’t be dealing with the same questions and we’ll be better prepared to deal with the challenge.”