
A malnourished child in Yemen waits with her mother for treatment at a humanitarian-aid centre.Credit: Essa Ahmed/AFP via Getty
As the devastation in Ukraine continues to unfold, many of the warnings about the global food crisis precipitated by the war have focused on the risks of famine and severe food insecurity. The Food and Agriculture Organization (FAO) of the United Nations, for instance, projected last month that between 8 million and 13 million more people could become undernourished in 2022–23 — meaning that they will be unable to acquire enough food to meet the daily minimum energy requirements over one year. There are already more than 800 million undernourished people globally1.
Another major concern is the possibility of severe price increases and disruptions to global systems for food, fertilizer and fuel, leading to millions more malnourished people in low- and middle-income countries (LMICs).
Women and children are particularly affected by the food shortages and high food prices resulting from the war against Ukraine. They are especially vulnerable to malnutrition: children’s nutritional needs are high relative to their body size, and women’s are high when pregnant or lactating. Furthermore, existing gender inequality and gender power imbalances — which can be exacerbated during crises — mean that women have less agency to direct resources towards feeding themselves and their children2. Lastly, these groups have already been disproportionally affected by the combined effects of other conflicts, climate change and the COVID-19 pandemic.
Broken bread — avert global wheat crisis caused by invasion of Ukraine
The impact of malnutrition might be less immediately visible than that of hunger. But left untreated, malnutrition can increase the risk of illness and death in the short term, and ultimately have multi-generational and irreversible effects. In fact, providing nutrition interventions in early life leads to extremely high estimated returns on investment — up to US$35 for every $1 spent3. This exceeds the returns on investment for other global health initiatives, including childhood vaccinations in the poorest countries — estimated in 2019 as saving $21 for every $1 spent4.
In mid-March, the FAO called on governments to avoid implementing restrictions that could hamper the global trade in food, fertilizer and fuel1. UN agencies are also urging governments to continue to expand various social protection programmes offered during the COVID-19 pandemic. These include the distribution of cash or food, or food vouchers for households in need1.
We applaud these efforts. But more is needed. Governments of LMICs, donors and other funders must invest now to safeguard people’s access to nutritious foods. Not doing so will mean immediate effects on child growth, development and immunity, and an increase in child deaths in the coming months. In the longer term, a global malnutrition crisis could lead to lifelong effects on education, diet-related chronic diseases and a decline in people’s capacity to thrive and contribute to their countries’ economic growth.
Crisis in context
Even before the COVID-19 pandemic, in 2019, 144 million children under 5 years old were stunted (meaning their height was low for their age), and 47 million had acute malnutrition, known as wasting5 (meaning their weight was low for their height). Meanwhile, 240 million women were underweight (with a body mass index of less than 18.5), and 468 million had anaemia6.
Record-high price hikes and disruptions in the trade of food, fertilizer and fuel (see ‘Price hikes’) threaten to further increase the global number of malnourished people, especially women and children, in three ways.
First, increased prices and reduced availability and access to food will directly affect the quality of people’s diets. Indeed, higher food prices disproportionately affect low-income countries, because their populations already spend a larger proportion of household income on food than do people in wealthy countries7.
Survey data collected during previous economic crises, such as in Indonesia and Bangladesh, indicate that when food prices rise, people maintain their consumption of calories by buying more highly processed foods, or cheap staples such as rice and maize (corn). And they reduce their consumption of more expensive nutritious foods, such as fruit, vegetables, meat and dairy8,9.

An unexploded missile in a wheat field in Ukraine.Credit: Vincenzo Circosta/ZUMA Press/Alamy
Children and women consuming unhealthy diets are at an increased risk of all forms of malnutrition (micronutrient deficiencies, wasting, stunting, becoming overweight) and ultimately of dying10,11. Women who have unhealthy diets are at a high risk of delivering babies of low birth weight, who are in turn likely to be malnourished early in life. And infants who don’t get the nutrients they need in their first 1,000 days (from conception to around two years of age) are more likely to be physically and cognitively impaired than are well-nourished infants. This means malnourished children have a greater risk of performing poorly at school and of being less economically productive in adulthood. It also makes them more likely as adults to have children who are malnourished — probably because of epigenetic effects during gestation12.
In many of the 50 countries that depend on grain imports from Ukraine and Russia, such as Pakistan and Egypt, more than 70% of the population could not afford a healthy diet even before the war1. Estimates suggest that the rising cost of staple grains and energy-related price increases for other foods, such as animal products and cooking oils, will further reduce the purchasing power of people in Pakistan and Egypt by about one-third. That would mean that 91% and 95% of those country’s populations, respectively, would not be able to afford a healthy diet1. (FAO estimates are subject to uncertainties, such as the duration of the war and its impact on planting season, the expansion of alternative food or fertilizer exporters, and the capacity of governments to mitigate the impact of increased consumer prices, for example through subsidies.)
Higher food and fuel prices might also result in households using health services less frequently and people spending less on soap and cleaning products. Poor hygiene further increases the risk of people becoming malnourished through conditions such as diarrhoea13. Less frequent visits to health providers can lead to reduced use of antenatal care, and less treatment for wasted or stunted children. Diarrhoea in children can both increase nutrient needs and disrupt the gut microbiome, making it harder for children to absorb whatever micronutrients are available.
What the war in Ukraine means for energy, climate and food
Second, price hikes and trade disruptions can increase the number of malnourished people by reducing the reach of humanitarian services that prevent and treat acute malnutrition.
These services include emergency food assistance in times of crisis (through the distribution of cash and food, such as flour, cereal, beans or lentils fortified with vitamins and minerals). They also cover routine interventions that prevent and treat acute malnutrition, such as the provision of fortified blended food cereals, and of specialized lipid-based supplements (such as ready-to-use products or therapeutic foods).
The costs of providing emergency food assistance, already up by 30–50% since 2019, are now escalating rapidly, while the price of foods specially formulated to treat and prevent child malnutrition increased by 10–20% between February and mid-March, according to unpublished data from the UN World Food Programme (WFP). In fact, even at pre-war commodity prices, the WFP, the UN children’s fund UNICEF and other partners could treat less than one in four of the children worldwide with acute malnutrition.
Finally, the war against Ukraine could prompt countries to reallocate their current budgets for improving people’s nutritional status to other areas.

People in Afghanistan help to transport sacks of flour from the World Food Programme.Credit: Scott Peterson/Getty
During the COVID-19 pandemic, more than 200 countries enacted social protection programmes targeted to poor populations14. The ongoing rise in prices presents significant fiscal challenges for many governments of LMICs in which national debts have already grown because of such programmes. Likewise, high-income countries could change their spending priorities, rather than increase their overall budgets for official development assistance. This might be especially true for some European countries that are facing both rising prices and one of the biggest refugee crises of modern times; more than ten million people in Ukraine have now been displaced from their homes.
Crisis upon a crisis
Unlike the last global food-price crisis, triggered by the financial crash of 2007–08, the current upheaval comes after governments and households have spent two years trying to cope with the COVID-19 pandemic — the worst economic shock since the Second World War. What’s more, many of the countries that are most vulnerable to the effects of escalating food and fuel prices are also dealing with conflicts (such as Ethiopia, Afghanistan, Myanmar and Yemen) and extreme climate events, including the drought that has afflicted East Africa since 2020. Both Ethiopia and Yemen are already facing the risk of famine because of drought and extended conflict.
Last year, the World Bank conservatively estimated that the COVID-19 pandemic led to an additional 97 million people being thrown into poverty in 2020, compared with 2019 (poverty is defined as living on less than $1.90 per day; see go.nature.com/3jebktj). This is a historically unprecedented increase.
Also last year, the Standing Together for Nutrition Consortium made similarly sobering estimates. (The consortium is a group of around 35 nutrition, economics, food and health-system experts, including 9 of us, established in 2020 to address nutrition challenges related to the COVID-19 pandemic.) Estimates included: 13.6 million more children with wasting by 2022, representing almost a 30% increase over 3 years (see ‘From bad to worse’); 3.6 million more children with stunting; 4.8 million more women with anaemia when pregnant5; and 141 million people added to the 3 billion who could not afford a healthy diet in 2019. The consortium also estimated that, by 2022, more than 1.5 billion people would not be able to afford even half of the cost of a healthy diet15.
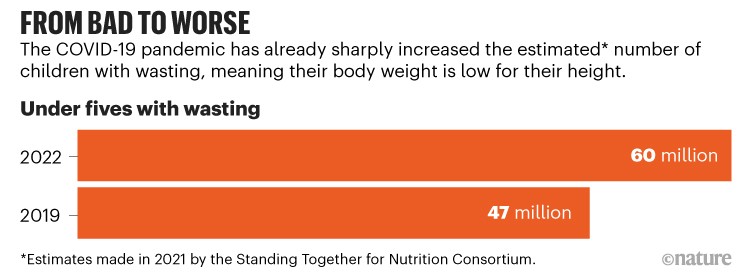
Source: Ref. 5
The WFP estimated in 2019 that 150 million people in 81 countries needed food assistance. By February (one month before the war against Ukraine), that had risen to 276 million people as a result of the combination of other conflicts and climate- and COVID-related shocks. The WFP expects that number to increase further this year, to 323 million.
Five urgent actions
We urge governments, donors and the United Nations to help to prevent a major exacerbation of malnutrition, especially for women and children. Global and regional political bodies can also play a part — among them, the World Trade Organization, the Association of Southeast Asian Nations, the South Asian Association for Regional Cooperation, the African Union, the G7 group of the world’s largest economies and the G20 group of 19 nations and the European Union.
Five actions are needed now.
End trade restrictions that affect access to nutrition. Globally, more than 15 countries, including LMICs such as Indonesia and Morocco, have implemented export bans to protect their own markets. Existing calls from the FAO and other trade and government organizations to reduce restrictions on global food and fertilizer must be heeded.
Governments should also prevent food hoarding, for instance by putting restrictions on the number of bags of cereal that traders or consumers can buy. During the global food crisis of 2007–08, prices increased in part because large food-producing countries, such as Thailand and Vietnam, restricted exports to preserve their domestic supplies and insulate their populations from higher prices16,17.
The war in Ukraine is exposing gaps in the world’s food-systems research
Sustain or implement social protection programmes. LMICs should build on the surge of measures brought in during the COVID-19 pandemic, and tailor them to address malnutrition in the most vulnerable people. Interventions could be in the form of food transfers, in which households receive packages that include staple grains, such as rice or flour fortified with micronutrients; vouchers that can be used only to purchase nutritious foods; or cash transfers. Even before the pandemic, cash transfers were well-established in LMICs as tools for increasing the ability of women to direct spending towards improving families’ diets and overall health18.
Innovative financing mechanisms might offer ways for countries struggling with debt to tap new funding sources — such as those from private foundations, or from investors seeking ways to incorporate environmental, social and governance factors into their investment decisions.
Protect national nutrition budgets. Last year, The Lancet’s Series on Maternal and Child Undernutrition Progress described several cost-effective and scalable interventions to address malnutrition in women and children (see go.nature.com/3ue7y19).
These include interventions, such as the use of specialized nutritious foods, to prevent and treat acute malnutrition or wasting in children; micronutrient supplements for pregnant women, young children and adolescents; and educational and other tools to promote, support and protect breastfeeding, and to encourage healthy diets and physical activity. Other interventions are the provision of meals at schools; large-scale food-fortification programmes, such as those involving the iodization of salt and the addition of vitamin A to cooking oils19; and breeding crops to have higher nutrient content (biofortification).
Governments of LMICs must continue to provide these proven nutrition interventions for women and children, particularly during the first 1,000 days of life.

Children in southern Madagascar waiting for food to be distributed in September 2021 after a drought caused a food crisis in the region.Credit: Frederic Lafargue/Paris Match via Getty
Honour commitments already made. In December 2021, 181 stakeholders, including 66 governments, attended the Nutrition for Growth (N4G) Summit in Tokyo. Driven by the urgency of the COVID-19 pandemic, these stakeholders committed a total of $27 billion in new funding to tackle food insecurity and malnutrition globally. The nearly 400 commitments made at the summit include a 40% reduction in stunting in children and a 50% reduction in anaemia in women of reproductive age by 2030 (see go.nature.com/3ebz98b).
If the world is to have any chance of reaching the UN Sustainable Development Goals — which include ending hunger, achieving food security and reducing all forms of malnutrition by 2030 — governments and donors must deliver on these commitments.
Mobilize more resources for humanitarian assistance. Urgent and critical humanitarian assistance for the Ukrainian population is being scaled up. At the same time, assistance for other populations affected by conflicts, the pandemic or climate change must continue and cannot be compromised.
In fact, much more funding is needed to address a rapidly worsening food-security and malnutrition crisis. The $27-billion investment promised at the N4G Summit is a good start. But in 2021, the Standing Together for Nutrition Consortium estimated that an additional $44 billion would be needed to address the challenges stemming from the COVID-19 pandemic alone. And that’s on top of the $70 billion over 10 years that the World Bank estimated in 2017 would be needed to achieve the global targets for reducing stunting in children and anaemia in women; for the exclusive use of breastfeeding during the first six months of every child’s life; and for the reduction of wasting in children.
Long term
Ultimately, governments, donors, the private sector and civil-society organizations — such as non-governmental groups and consumer and trade bodies — must help to build food systems that are more resilient and sustainable, and that support people’s consumption of safe, nutritious and affordable diets.
This can be done by using more diverse and environmentally sustainable food-production systems; by reducing waste at every level of the supply chain, from production to distribution and consumption; by improving transport, processing and storage such that the nutritional value of the food is retained; and by enacting policies and creating environments that foster healthy diets20,21. The latter can be done by improving the quality of publicly distributed food — for example by using fortified and fresh foods, or by using vouchers specifically for nutritious food22.
Also of crucial importance are timely, standardized nutrition data to guide policy and funding. Two years into the COVID-19 pandemic, no global monitoring data exist to reveal the impact of the pandemic on women and children’s nutritional status.
Technological advances, such as modelling approaches that use proxy indicators to identify whether people are eating healthy diets, offer tremendous opportunities. Too often, data-monitoring systems focus on upstream indicators, such as poverty, food security or food prices. These are relatively easy to measure, even in a crisis. But it is a child’s weight or feeding practices, or a woman’s diet or the levels of micronutrients in her blood, that can provide an early warning of faltering growth and malnutrition risk.
Investing in more and better data could significantly reduce the costs of food-assistance programmes and increase the number of people reached. For example, in 2015, researchers used an economic-optimization tool to identify the most cost-effective package of vitamin A interventions for regions in Cameroon. (Potential approaches included giving people vitamin A supplements, and fortifying cooking oil or stock cubes.) Overall, the programmes suggested by the optimization tool were about 44% less expensive than blanket, nationwide programmes23.
In summary, beyond the immediate problem of food shortages, the current crisis could affect a generation of women and children who are already vulnerable to malnutrition — with implications for the human capital of communities and nations spanning generations.
Now is the time to redouble efforts to ensure that the world’s women and children get the food and nutrition they need.

 What the war in Ukraine means for energy, climate and food
What the war in Ukraine means for energy, climate and food
 The war in Ukraine is exposing gaps in the world’s food-systems research
The war in Ukraine is exposing gaps in the world’s food-systems research
 Broken bread — avert global wheat crisis caused by invasion of Ukraine
Broken bread — avert global wheat crisis caused by invasion of Ukraine








